Research
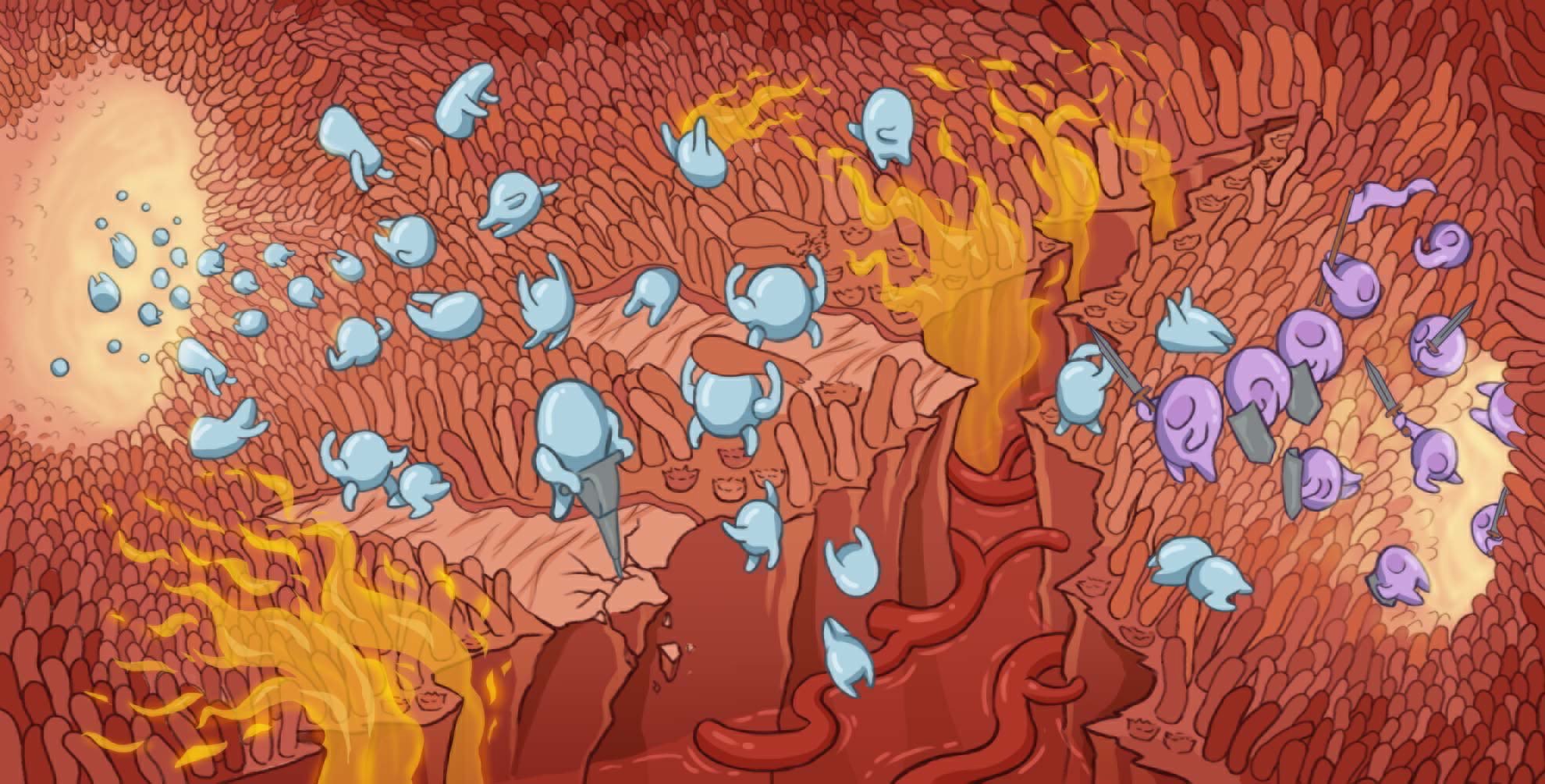
Our research aims at understanding the molecular mechanisms regulating gut homeostasis: i.e. finely tuned balance between response against enteric pathogens vs. tolerance of commensals. For this, we employ an integrative system approach by combining stem cell biology, virology, genomics, bioengineering, and cell biology to dissect host/pathogen interactions at the intestinal mucosa surface.
Our long-term goal is to develop technologies and cross disciplinary pipelines to tailor pharmacological interventions to both the host (patient specific, cell type specific or pathology specific) and the pathogen (norovirus, coronavirus, rotavirus, astrovirus).



